Ok, so it is time to put together the previous two parts of this series and figure out what they give us (if anything). Let’s recap:
In part 1, I introduced the issue at hand: I am stressed and anxious a lot of the time, but I feel unsatisfied by advice about “living in the moment,” and shifting away from an achievement oriented mindset. It feels like not making the most of my life. It feels like giving up and settling for mediocrity. That led to the question of what I actually mean when I talk about making the most of life, which required some definitions.
The starting point is that all humans have intrinsic rights and worth. You don’t have to do anything extra to deserve food, shelter, health, education, love, happiness, and fulfillment. I also talked about how “doing good” is actually awfully hard to pin down and basically you just have to do what you can to make the world a nicer place, within reason. If you start to overthink it, you quickly end up paralyzed (see also: Chidi Anagonye in The Good Place).
Achievement is not inherently good, but achieving goals that are personally fulfilling is a great thing to do as long as those goals don’t harm others. And meaning? There is no meaning but what you make it.
In part 2, I realized that my answer to what it looks like to spend your life well boils down to three “simple” parts: do good, create something, and have fun. Sounds good, right?
My first instinct for part 3 of the series was to go through the three things from part 2 and evaluate how well I am doing them in my life and where I could improve. I wrote a bunch about it, but it felt… wrong. Something was off. Probably you already can see what took me way too long to realize. I think parts 1 and 2 have some pretty good stuff in them, but there’s a fundamental flaw. The problem with trying to figure out how to “spend your life well” is that it immediately leads to trying to measure up your life against some standard.
If the definition of a life well spent is that you Do Good, Create Something, and Have Fun, then how much is enough? How much good do I need to do? How much do I need to create? How much do I need to enjoy myself? What is the best balance of the three? There’s no answer. This is the whole point of The Good Place, and despite (I thought) understanding that point, I somehow ended up making the same mistake, but with two extra dimensions. Because why settle for beating myself up over just one thing when I can beat myself up over three?
If there is no such thing as “enough” good/creativity/enjoyment to make a life qualify as “well spent” that means one of two things. On the one hand, maybe it’s an impossible goal to reach and no matter what I do I’ll always be dissatisfied, because I could always be doing more.
Or on the other hand, maybe there’s no such thing as “enough” because there is no need to do more. I’ve already done enough. Everyone has. Because, to circle back to the quote from Part 1:
“Here’s a secret I tell to my students. I’m going to tell it to you. You aren’t a tool. You are an end in yourself. Meeting your personal goal, whatever that might be, won’t give you one iota more worth than you already have. The purpose you hope to serve will hopefully fulfill you, but has no effect on your worth.
Human worth is contingent upon nothing, and your dreams are separate entities from you.”
It turns out that quote is not the only place I’ve heard this message. In the book Feeling Good, which I read several years ago – the one that partly inspired my Finding Balance posts – I not only read but highlighted the following:
“Essentially, you must acknowledge that human “worth” is just an abstraction; it doesn’t exist. […] Therefore, you cannot have it or fail to have it, and it cannot be measured. Worth is not a “thing,” it is just a global concept. It is so generalized it has no concrete practical meaning. Nor is it a useful and enhancing concept. It is simply self-defeating. It doesn’t do you any good. It only causes suffering and misery. So rid yourself immediately of any claim to being “worthy,” and you’ll never have to measure up again or fear being “worthless.” Realize that “worthy” and “worthless” are just empty concepts when applied to a human being.”
[…]
“Rather than grasp for “worth,” aim for satisfaction, pleasure, learning, mastery, personal growth and communication with others every day of your life. Set realistic goals for yourself and work toward them. I think you will find this so abundantly gratifying you’ll forget all about “worth,” which in the last analysis has no more buying power than fool’s gold.“
[…]
““But I’m a humanistic or spiritual person,” you might argue. “I’ve always been taught that all human beings have worth, and I just don’t want to give up this concept.” Very well, if you want to look at it that way, I’ll agree with you, and this brings us to the second path to self-esteem. Acknowledge that everyone has one “unit of worth” from the time they are born until the time they die. As an infant you may achieve very little, and yet you are still precious and worthwhile. And when you are old or ill, relaxed or asleep, or just doing “nothing,” you still have “worth.” Your “unit of worth” can’t be measured and can never change, and it is the same for everyone. During your lifetime, you can enhance your happiness and satisfaction through productive living, or you can act in a destructive manner and make yourself miserable. But your “unit of worth” is always there, along with your potential for self-esteem and joy. Since you can’t measure it or change it, there is no point in dealing with it or being concerned about it.”
– Feeling Good, David Burns
I claimed up front that I agreed with this idea, and then spent a whole lot of time and mental energy essentially tricking myself into coming up with a way to judge a life’s worth without admitting what I was actually doing. Because if I say that there are better or worse ways to spend one’s life, that’s just a different way of saying that if you spend your life “well” then your life has more worth.
So where does that leave us after all of this existential ruminating? I stand by my three facets of a life well spent: Do Good, Create Something, Have Fun. I think that’s a pretty solid framework. But the error that I made when I first started to write this Part 3 post was to treat the three facets like a report card: metrics to be tracked and judged acceptable (or not) as if there was such a thing as an existential FitBit. (“You’ve hit your daily goal of 5,000 Fun Units, but you are only at 2,000 Doing Good units and 3,000 Create Something units!”) This tendency to measure and evaluate everything is a habit of mind that comes from years of training as a scientist combined with a broader cultural bias toward the quantitative over the qualitative even in extremely qualitative contexts like philosophy.
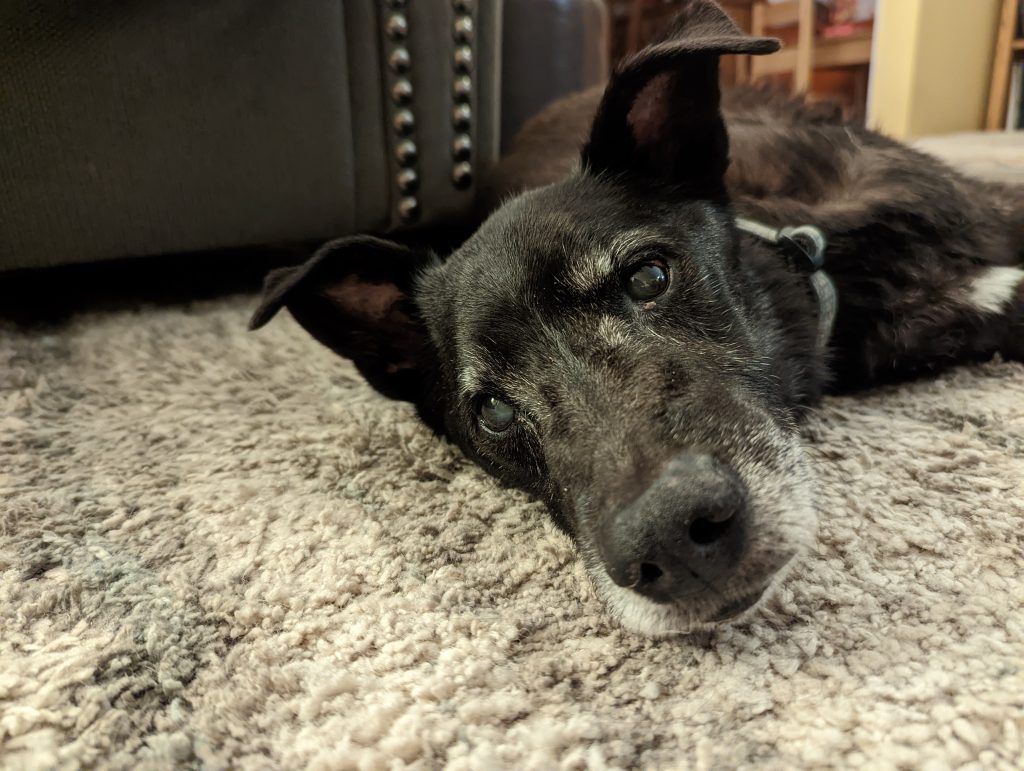
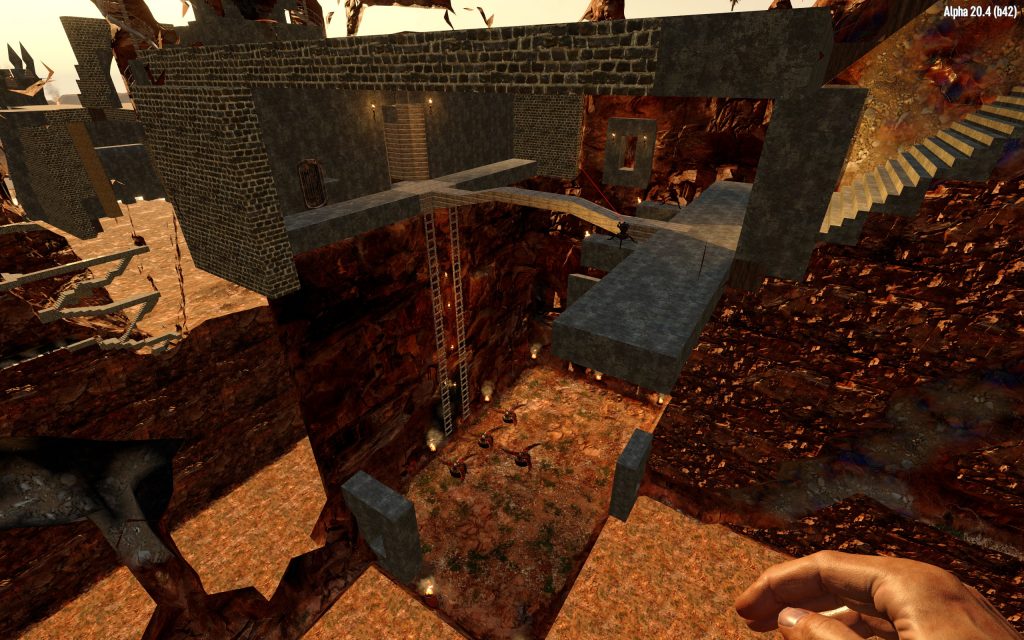
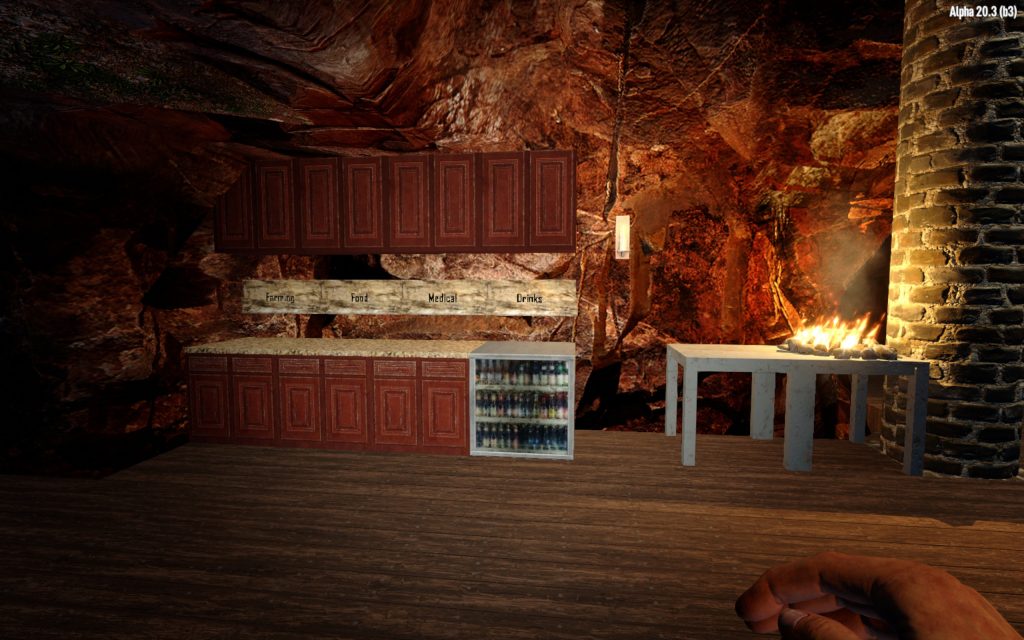
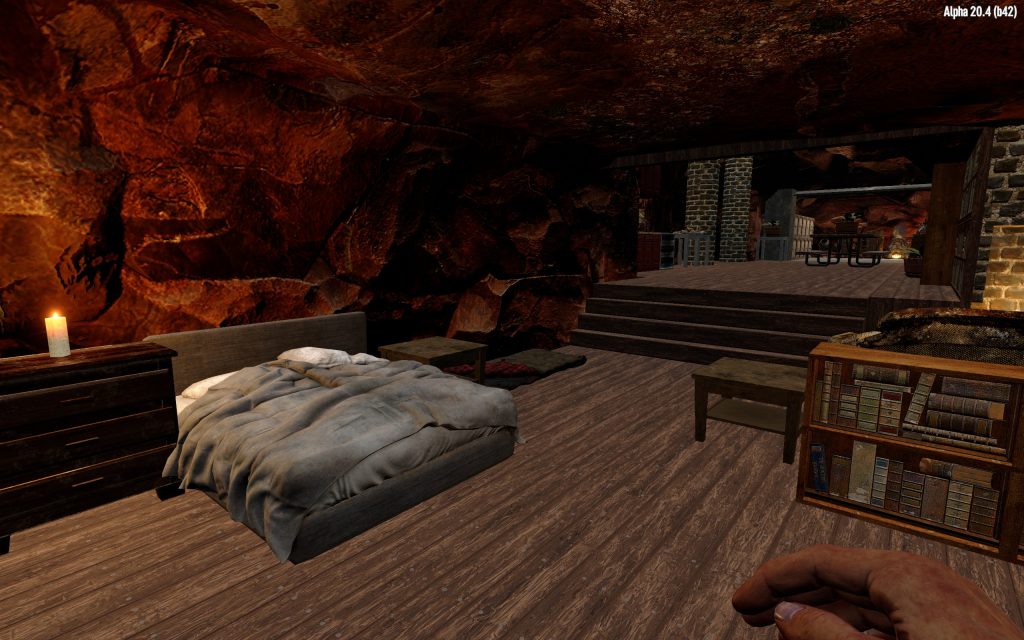
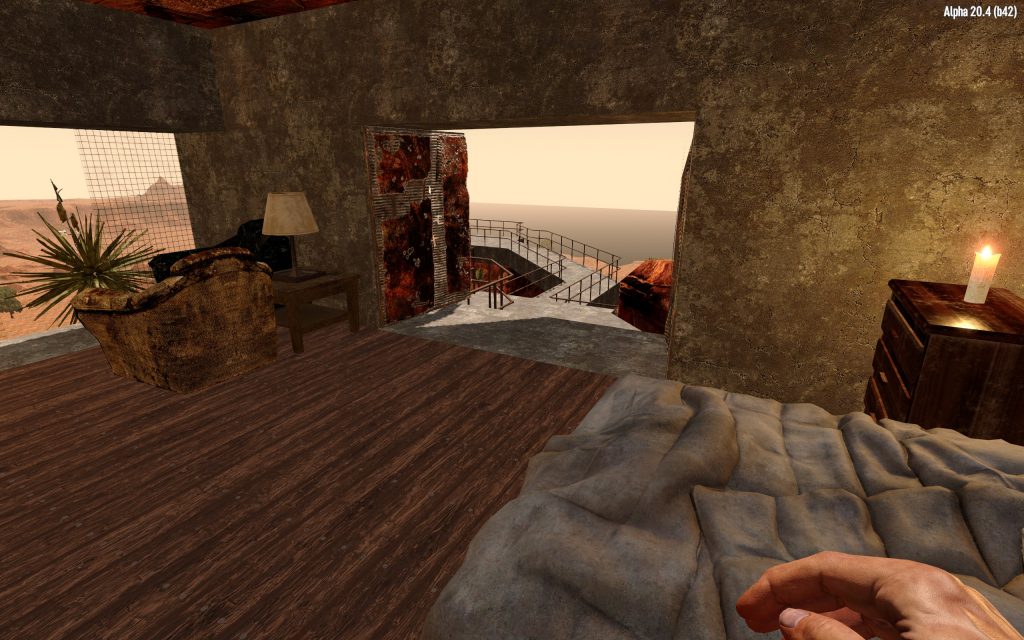
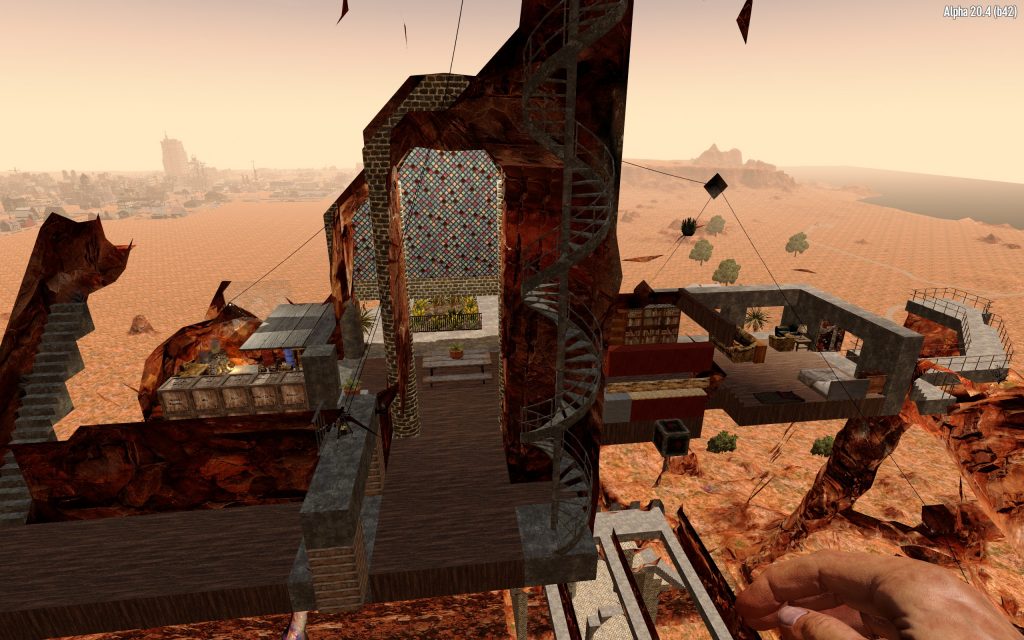
What if rather than trying to quantify the three metrics, which tends to result in beating myself up for not doing enough, I just took them as guides? If I’m feeling anxious or down or dissatisfied, check in with the three facets. Maybe I’ve been working all day and I feel crummy because it feels esoteric and pointless. Maybe it’s time to Do Good and participate in a protest or evaluate my charitable giving or volunteer. Maybe I’m depressed by the state of the world and the fact that no matter how much I donate or volunteer, I can’t overcome the outside forces that seem hellbent on steering society toward multiple interconnected simultaneous catastrophes. So that means it’s time to take a break and Have Fun going to the park with my family or playing a video game with friends, or Create Something by writing or painting.
Or even better than checking in with the three facets in response to how I’m currently feeling, make a conscious effort to structure my life in such a way that I feel good about all three. Some of this may be changing my actions, and some of it may be reframing what I’m already doing. Both are good!
Let’s return to the fundamental problem that led me to start these posts: Why do I feel unsatisfied with all of this self-care type advice about intrinsic worth, living in the moment, not focusing on being “productive”, etc.? A big part of it is just the society we live in. I grew up in a capitalist and individualist culture that prizes a “Protestant work ethic” surrounded by other high achievers. It’s impossible for that not to shape my thoughts and values at a very deep level.
I spent all of my 20s striving for more responsibility as I climbed the academic ladder. As I discussed before, graduate school takes people who are already extremely focused on achievement and external validation, and then amplifies those tendencies to a pathological degree (pun intended).
After I finished graduate school and got a permanent position at USGS, I realized that I had “made it” and didn’t want to climb any further. That way led to supervisory responsibilities (i.e. even more bureaucracy) and/or leadership on spacecraft instruments which is not compatible with the work life balance that I wanted, especially once we had kids.
So the theme of my 30s was trying to cut down on responsibilities. Not taking on new projects, turning down opportunities that would have advanced my career further, shying away from “hot” research topics in favor of something specialized without much competition, not adding things to my plate, avoiding things both at work and in my personal life that require too much planning and logistics, even (for the last few years) reducing my hours at work in an effort to somehow get to the point where life does not feel overwhelming. To escape the feeling of constantly treading water and struggling to keep my head up.
It has, in short, not worked. I have reduced my work responsibilities, but what is left still stresses me out. Nothing is ever finished. There’s always another issue, another change, another revision. Someone always has a special case to be dealt with, or wants to revisit something that was discussed and decided years ago. And I have increasingly lost the spark of inspiration that led me to space exploration. This probably deserves its own post, but the short version is that given the current state of the world, it is hard to feel really passionate about improving the accuracy of chemical measurements in rocks on Mars by a fraction of a percent. This is something I have always struggled with, but since 2016 – when I both became a parent and our country elected the worst possible person to the presidency – that struggle has gotten significantly harder. It’s as if a part of my mind is constantly whispering in my ear: How dare you, with all of your privileges, dedicate your life to something that doesn’t help others? (Yes, I know, it’s a false choice. Fundamental science is important even if it isn’t immediately helpful, etc. I know all the arguments. But people still suffer and die and the world falls apart while I have backed myself into a corner where my work is esoteric even to those scientists who use my results to do their own esoteric research.)
All of that to say that I have found myself mentally withdrawing from work for years, and have not done a very good job of filling that void.
I keep coming back to this quote from Man’s Search for Meaning that I shared in Part 1:
“What man actually needs is not a tensionless state but rather the striving and struggling for some goal worthy of him. What he needs is not the discharge of tension at all costs, but the call of a potential meaning waiting to be fulfilled by him.”
I think my fundamental mistake has been interpreting all the feel-good self-care advice as telling me to do less. I don’t just need to pause and breathe. It’s not satisfying to be told that I don’t need to do anything because my worth is not contingent. I don’t need more idle time, I need more meaningful time. “Living in the moment” or “finding balance” or accepting that all humans have intrinsic worth does not mean that I need to do less to be happy. When I do nothing, I feel restless and anxious. It is times when I am busy with something that I enjoy and am passionate about that I feel the best.
This is the true joy in life, the being used for a purpose recognized by yourself as a mighty one; the being thoroughly worn out before you are thrown on the scrap heap; the being a force of nature instead of a feverish selfish little clod of ailments and grievances complaining that the world will not devote itself to making you happy. -George Bernard Shaw
So what I really need to do is find myself a new goal or goals. The trick is, I don’t want to fall into the trap of the achievement-based mindset. If I pour all of my passion an energy into a specific project, what happens when that project ends? Kieran Setiya argues that what we call a “midlife crisis” often stems from relying too much on “telic” activities for fulfillment. A “telic” activity is one with a specific goal and end point built-in. Finishing a project. Reaching a destination. Get a PhD. Reaching the point in one’s career where there is no next degree or promotion or milestone to reach and instead you face decades of basically the same work day after day…
Setiyah argues that the key to fulfillment in life is to focus more on “atelic” activities:
“We can escape the self-destructive cycle of pursuit, resolution, and renewal, of attainments achieved or unachieved. The way out is to find sufficient value in atelic activities, activities that have no point of conclusion or limit, ones whose fulfillment lies in the moment of action itself. To draw meaning from such activities is to live in the present – at least in one sense of that loaded phrase – and so to free oneself from the tyranny of projects that plateau us around midlife.”
― Kieran Setiya, Midlife: A Philosophical Guide
One atelic activity that appeals to me is writing. It’s a little tricky because individual writing projects (e.g. a novel, or, say, a series of philosophical blog posts) are telic. You write the thing, and then it is done. But the process of writing, of developing the skill of capturing thought and feeling in written words, that is an atelic activity. Its “fulfillment lies in the moment of action itself.” You can do it forever, and continue to improve, and always seek that flow state where the world drops away.
Once you start writing, it is fatal to think about anything but the writing. True work is done for the sake of doing it. – Ursula K. LeGuin
Another is art. I used to draw all the time as a kid. A couple years ago I took a watercolor class, and although I have only painted a few times since, it is a very reliable way to drop into a flow state. It makes my brain happy. Like writing, individual projects are finite, but the process, developing the skill, the act of painting, is atelic and very rewarding.
So I’d like to do more writing and art. I also want to find some organization or cause that I believe in and can support with my time and effort. This one will take some time to figure out, but I think it is a missing piece of the puzzle. Setiya argues that if there is anything like a “meaning of life” it is basically to do what you can to make the world a better place:
“…the goal to which we should aspire, and for which we strive together, is a world in which people are as happy as they deserve to be. […] All we can hope for is progress towards justice, ever imperfect, but sufficient to give meaning to human life.”
– Kieran Setiya, The Meaning of it All
Where I get stuck, whether it is in writing, or art, or volunteering is that my mind tends to aim too big. I don’t just want to write, I want to write a bestselling novel! I don’t just want to play around with color mixing, I want to perfectly capture that feeling or image in watercolor that I would want to hang on my wall! I don’t just want to donate to charity to treat symptoms, I want to fix the root cause of the problem! The quotes I included above play into this, they make it seem like I need to find a single source of meaning, to strive and struggle for one specific worthy goal, and “a purpose recognized by yourself as a mighty one”
So I get paralyzed. I put too much pressure on doing the best thing and end up doing nothing. I don’t write. I don’t paint. I don’t volunteer. And then I beat myself up about it and feel dissatisfied.
It’s worth revisiting the quote from the previous post, where Setiya talks about how we can never be sure we have done enough (emphasis added):
[We shouldn’t condemn] our own efforts as too small. They may be small—but it’s perverse to deal with that by throwing up our hands and doing less. There is value in a single step toward justice, and one step leads to another.
[…]
You may not do enough, but the difference you make when you save a life is the same whether you save one of two or one of two million.
Or, famously:
Perfect is the enemy of good.
I think this is the missing piece. I need to stop getting paralyzed by the thought that whatever I do isn’t enough, because that paralysis prevents me from doing anything, even something small. It’s better to do something small than nothing at all.
So as I wrap up this series of posts, and as we begin the new year and make resolutions, here is what I will be focusing on.
First, the three aspects of a good life that I cam up with in Part 2. And second, a shift in focus from the telic to the atelic and from the big to the small. No more paralysis, no second guessing whether what I am doing is enough. Instead, small steps. If I want to write, start with something I can finish in a day or a week instead of a novel. If I want to paint, give myself permission to just mess around, don’t try to immediately produce a masterpiece. If I want to volunteer or donate, then don’t get caught up in whether what I’m doing is the best possible thing. Just do something.
Do Good.
Create Something.
Have Fun.
Find fulfillment in the action itself.
There is value in a single step.